It is hard to overstate the importance of the moment. For billions of years, life on Earth has been shaped, slowly and incrementally, by dumb evolution. But in research this week, scientists showed how that might change. With advanced genetic engineering tools, a US-Korean team mended dangerous heart disease mutations in human embryos for the first time. The feat paves the way for radical new treatments – and for humans to take control of their genetic destiny.
The ability to edit human genomes may one day transform people’s lives, but in breaking new ground, it would cross a line that has long been controversial. Today, many countries prohibit the creation of genetically altered people, even if the procedure would spare them a devastating and life-shortening disease. The caution comes from the fact that changes to an embryo’s DNA affect not only the child in question, but their sperm or eggs. When the time came, they would pass on the modifications – and any harmful side-effects the procedure may cause – to their children and future generations.
The risk of causing unintended harm to unknown numbers of people is only one concern. Inevitably, the ability to tweak the DNA of unborn children raises the prospect of designer babies. There are broader fears too: that eradicating certain mutations could threaten people’s identities, and even the sense of what it means to be human. “If we change our DNA forever, are we still human? I think we are a lot more than our DNA, but people have different answers to that question,” said Christine Watson, professor of cell and cancer biology at Cambridge.
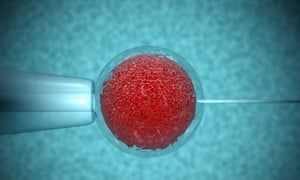
The work by the US and Korean team is a milestone. Around the world, a handful of groups are exploring how to correct faulty genes in human embryos in the hope of preventing terrible diseases from being passed on. Until now, all have come up against the same brick walls. Having treated embryos for harmful mutations, tests reveal that some still linger, leading to what are called “mosaic” embryos. Another common glitch is that the very procedure meant to fix bad mutations causes fresh ones elsewhere, producing so-called “off-target effects” and posing a cancer risk. The researchers overcame both these hurdles by performing the editing procedure when the sperm and egg first met.
“The big step forward is that they managed to correct the mutation, have a very low level of mosaic embryos, and seemingly no off-target effects,” said Watson. “That for me is the big safety concern: that by correcting one mutation you introduce another and who knows what that might do.”
At face value, the research has enormous potential. More than 10,000 inherited diseases might be prevented by correcting harmful mutations. Many of them are serious, such as Tay-Sachs, cystic fibrosis, Huntington’s disease, and breast cancer linked to mutations in the BRCA gene. But in reality, very few people would benefit if existing bans on genetically altered embryos were suddenly lifted. In the majority of cases, people who know they carry a heritable disease, and who want genetically-related children, can go through IVF and have their embryos screened for harmful mutations. Fertility doctors do this every day and select only the healthiest embryos to implant in prospective mothers.
In their study, the US-Korean team showed that genome editing could boost the number of embryos free from heart disease mutations from 50% to 72%. In the clinic, that would give doctors more healthy embryos to choose from. But as Tom Shakespeare, professor of disability research at Norwich Medical School, points out, it doesn’t help parents dramatically. “As of now, what’s been achieved is no better than what we already have. If I have a 50% chance of passing on my condition, and then I have a complex procedure that lowers that to 28%, it hasn’t solved the problem,” he said.
There are situations where embryo screening cannot work, and where genome editing could help. The classic example is a person who carries two copies of the mutation that causes Huntington’s disease. Every embryo created from their sperm or eggs would carry at least one disease gene, enough for the condition to take hold. In this case, genome editing could help by overwriting the Huntington’s mutation with a functional copy of the gene. But the number of people who carry two Huntington’s genes is vanishingly rare, measured in the dozens worldwide.
“We are really talking about a very, very small set of people and it’s easy to forget that because the science is so exciting,” said Karen Yeung, director of the Centre for Technology, Ethics and Law in Society at King’s College London and chair of the Nuffield Council on Bioethics Working Group on Genome Editing and Human Reproduction. One of the issues ethicists still grapple with is how to weigh up the common desire for people to have genetically-related children rather than adopt or simply have no children.
A more effective way to reduce genetic disease could be a national genetic testing program that identifies people who are carriers of harmful genes and at risk of passing them on. “I think the only way we’ll make progress with genome editing is when sequencing is cheap enough that every baby will have their genome sequenced at birth,” said Watson. “It’s going to be cheap enough to do that soon, but will people think it’s acceptable?”
In the UK it is illegal to implant a genetically altered embryo in a woman, and regulators in the US and other countries disallow the procedure. The situation is unlikely to change soon, according to Chris Gyngell, a bioethicist at Oxford. “I don’t think there’s going to be strong political will to change the law in the next few years, and probably not until babies are born elsewhere in the world that turn out to be fit and healthy.”
One of the barriers to lifting the ban is that genes, and therefore the risks of altering them, are so poorly understood. Genes rarely have only one job in the body, so a change here can cause an unexpected effect elsewhere. One dual role that is known about comes from HIV research, where people with mutations in the CCR5 gene are resistant to HIV, but more susceptible to West Nile virus. But plenty of other genes are not so well understood.
With all the risks inherent in genome editing, Shakespeare is not convinced that there will be a huge demand for designer babies, even if the many genes that influence traits like intelligence and a sparkling personality are ever found. “Behavioural genetics is so complicated,” he said. “I’d say environment will be far more important than genetics for the foreseeable future. You can see from the current cabinet that it doesn’t matter how intelligent you are, it matters what school you went to.”










